What is Sharpe’s Syndrome?
Mixed connective tissue disease (SSTF), described as an independent rheumatic disease relatively recently, in accordance with the classical ideas of its nosological autonomy, is characterized by a combination of clinical signs characteristic of SLE, systemic scleroderma, RA, and dermatomyositis in combination with a high titer of antibodies to nuclear ribonucleoprotein in serum blood. The authors of the first descriptions of this disease also stressed that the rarity of kidney damage, the effectiveness of treatment with corticosteroids and a generally relatively favorable prognosis can be attributed to its characteristic features.
Although the combined forms of the diseases listed above were seriously analyzed long before the relevant works of G. Sharp, the peculiarity of this author’s approach was the priority of immunological criteria. Essentially, the initial basis for the allocation of NWPC as an independent unit was not so much the combination of clinical symptoms of various DBSTs as the frequent detection of antibodies to a specific nuclear ribonucleoprotein (NRNP) with antigenic properties, which is destroyed by RNase and detected in the thymus gland salt, in the respective patients. In the literature, it is often also described under the name soluble nuclear antigen, or Mo-antigen. It must be emphasized that the determination of antibodies to nRNP requires a high immunological qualification, since, prior to analysis, it is necessary to separate nRNP from other antigens contained in the thymus gland extract. This extract contains more than 15 antigens, 6 of them are of great importance for rheumatology, occurring with the mentioned rheumatic diseases with a significant frequency (not less than 20%), which was confirmed by verification studies in various research centers.
The specific determination of antibodies to nRNP is carried out by various methods – immunofluorescence, hemagglutination and counter immuno electrophoresis.
In the first publications, it was reported that antibodies to nRNP are a specific laboratory symptom of FHTC, making it easy to navigate the diagnosis. It was indicated, in particular, that these antibodies were not only detected in almost 100% of patients with FHSCH, but were also absent in 398 out of 400 control sera. Subsequent observations, however, disproved the idea of the NWPC as the only rheumatic disease, which can be diagnosed using a single immunological indicator. In modern guidelines on rheumatic diseases, the NWPC acts mainly as a clinical concept with characteristic, but by no means specific, immunological features.
NWPC often occurs in people over 30 years old (average age around 37 years). Women suffer 4 times more often than men. In accordance with the title draws attention to the multiplicity and diversity of symptoms.
Symptoms of Sharpe’s Syndrome
It is often noted that it has been the first signs of the NWSD that it has been. with mottled type of luminescence in serum. In the future, there has been a certainty, it has not been possible, but it’s not possible.
Damage to the joints. Arthralgia occurs in almost all patients NWPC patients, and true arthritis is more than half. In most cases, the symmetric arthritis of the proximal interphalangeal, metacarpophalangeal, radiocarpal, knee and elbow joints is noted. The sproiliac joints are almost always absent. It is less severe than with RA. Serious deformities are relatively rare, although osteoporosis and slight erosion, sometimes asymmetrical, are relatively rare. It is found that it is aggravated by the RF.
Muscle impairment in patients with SSTF is characterized by weakness in the proximal extremities in combination with spontaneous or palpatory tenderness or without it. These phenomena occur in approximately half of the patients. There can be an increase in the level of creatine phosphokinase and aldolase. Electromyogram in such cases is typical for inflammatory myopathies; biopsy reveals degenerative changes in muscle fibers, interstitial and perivascular infiltration. It is a fact that the skin picture is indistinguishable from dermatomyositis.
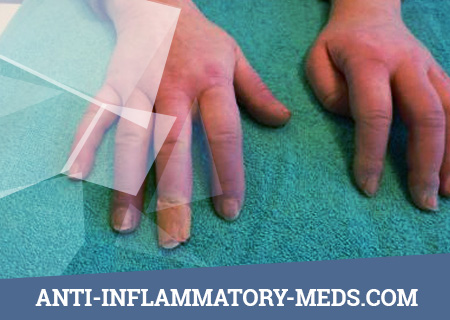
Raynaud’s syndrome is often the first sign of a FHCC. In some patients, it is very difficult. In rare cases, it is a vasculitis (“digital vasculitis”), which is indistinguishable from RA in RA.
It has been noted that many studies have not been observed. Even with isolated (“idiopathic”) Raynaud’s syndrome, 30% of patients. It has been suggested that the authors of the FCCT have been approved.
Skin changes. Approximately 70% of patients with SSTPs show swelling of the hands, and therefore the fingers have the appearance of thickened and sometimes somewhat tapering towards the end. The skin at the same time is tense and thickened; her biopsy reveals an increase in collagen and swelling. Such changes, very reminiscent of scleroderma, can reach significant severity, but nevertheless diffuse sclerosis of the skin, its merging with the underlying tissues, the formation of fibrous contractures and soft tissue calcification are observed. Ischemic necrosis and ulceration of the fingertips typical of classical scleroderma are equally rare. Very frequent (up to 40%) are chronic, accompanied by non-coarse cicatrization rash type discoid lupus erythematosus, as well as non-scarring diffuse erythematous rash (including on the face), resembling that of SLE. Similarly, erythematous patches over the metacarpophalangeal and prokalamic interphalangeal joints and especially the purple eyelid edema are essentially identical to the corresponding skin changes in dermatomyositis. Less frequent skin pathologies observed in patients with NWPC include hypertext or hypopigmentation, telangiectasia on the face and hands (including around the nail bed), and diffuse alopecia.
Renal pathology. The creators of the NWPC concept believe that the kidneys in this disease are rarely affected (about 10%), and in the event of the development of renal changes they are not pronounced. Using a biopsy, mesangial proliferative changes or membrane-proliferative nephritis are usually established. R. Bennett and B. Spargo suggested that it is the prevalence of membranous nephropathy that is the reason for the relatively good prognosis of patients with SSTFs with kidney damage, since even with SLE, membranous nephritis has a relatively favorable course. Nevertheless, descriptions of SSTP patients who died of progressive renal failure are known.
Lung lesions are rarely of clinical significance, although with targeted research, functional disorders such as decreased diffusion capacity and reduced tidal volume are established in most patients. Radiography often reveals signs of interstitial pneumonia, exudate in the pleura and pleural adhesions. The severity of these changes is usually quite modest, and only in some patients pulmonary manifestations with characteristic complaints (cough, shortness of breath) come to the fore. They are believed to be based on fibrosing alveolitis.
Cardiac disorders are less common than pulmonary pathology. The most serious of these is exudative pericarditis, which in some patients is interpreted incorrectly (in particular, as viral). Also described are myocarditis, leading to circulatory failure, and aortic valve insufficiency. Histological examination of patients’ hearts; who had no clinical signs of cardiac pathology during their lifetime, in some cases they detected areas of myocardial necrosis, interstitial and perivascular inflammatory infiltrates, fibrosis of the interstitial tissue, intimal thickening and narrowing of the lumen of a part of small vessels.
The digestive system and abdominal organs. Functional disorders of the esophagus, established using special methods (in particular, esophagomanometry), were found in 80% of patients. There was a decrease in peristalsis in the lower esophagus, a decrease in pressure of the upper and lower sphincter. In most patients, these disorders do not have a real meaning and do not cause any complaints, remaining only a purely instrumental functional indicator.
The intestine is rarely involved in the process. Peristalsis is reduced, colicky pains, bloating, alternating diarrhea and constipation, a syndrome of insufficient absorption, i.e., symptoms characteristic of systemic scleroderma, are noted. Cases of intestinal perforation are known.
Perhaps a slight increase in the liver, but its functions are not impaired. Rarely increases spleen.
Other clinical manifestations. Among other symptoms of SSTP, it should be noted first of all lymphadenopathy, which occurs in 1/3 of patients, which in some cases is so severe that it simulates malignant lymphoma. Approximately 10% of patients have trigeminal neuralgia. In isolated cases, SZCT revealed Sjogren’s syndrome and Hashimoto’s thyroiditis.
Diagnosis of Sharpe’s Syndrome
The combination of symptoms, to varying degrees inherent in various DBST, explains the diagnostic difficulties in recognizing FHTC. The first diagnosis is often wrong and is determined by the prevailing clinical signs. Thus, the combination of Raynaud’s syndrome with swelling and thickening of the skin of the hands naturally causes the idea of the onset of systemic scleroderma. Weakness in the proximal muscles of the extremities leads to the suggestion of polymyositis (dermatomyositis), which seems particularly justified with the simultaneous presence of skin lesions, first of all, swelling of the skin of the eyelids with a violet hue. Pleurisy, pericarditis, arthritis or arthralgia, accompanied by erythematous skin rashes and fever, lead to the diagnosis of SLE. Chronic recurrent symmetrical polyarthritis, while detecting in the serum of the RF, may lead the doctor to a diagnosis of RA.
The principles of differential diagnosis of FHDDs demonstrate the comparative frequency of the most important symptoms in FHEFs and clinically related diseases. Thus, the NWPC is distinguished from SLE by the high frequency of Raynaud’s syndrome, swelling of the hands, myositis, reduction of the motility of the esophagus, lung lesions and, conversely, the low frequency of severe kidney and CNS damage, LE cells, antibodies to native DNA and Sm, hypocomplementemia. The main differences of SSTF from systemic scleroderma are a significant incidence of arthritis, myositis, lymphadenopathy, leukopenia, hypergammaglobulinemia and a great rarity of diffuse sclerosis of the skin. Compared with polymyositis, NWRS to a much greater extent are characteristic of Raynaud’s syndrome, arthritis, swelling of the hands, lung damage, lymphadenopathy, leukopenia and hyperglobulinemia. The assumption of a possible FHST should be discussed in cases where the symptoms characteristic of it and the symptoms discussed above occur in patients whose disease was previously treated as SLE, scleroderma, polymyositis, Sjogren’s syndrome, chronic active hepatitis, vasculitis, viral pericarditis, Verlhof syndrome. Naturally, in such situations it is necessary to determine as quickly as possible antibodies to RNP, the presence of which is so essential for the diagnosis of FHTC.
Sharpe’s Syndrome Treatment
The features of NWPC usually include the favorable effect of corticosteroids on the main manifestations of the disease. Mild forms of the disease are often successfully treated with small doses of prednisone, and in some cases only NSAIDs. In severe organ lesions, high initial doses of prednisolone (up to 1 mg / kg body weight) are recommended, which in these situations give a particularly fast and complete effect with the possibility of reducing the daily dose in a relatively short period of time compared with the corresponding tactics in classical forms of SLE or systemic scleroderma. Significant positive dynamics of arthritis, myositis, serositis, skin rashes, hepato and splenomegaly, lymphadenopathy, anemia and leukopenia, as well as the normalization of body temperature is achieved after the start of adequate hormonal therapy in a short time (from several days to several weeks), after which you can gradually decrease dose of steroids to a small supporting or until the complete abolition. G. Sharp (1981) notes that as a result of these approaches to treatment, most patients can return to a normal or almost normal lifestyle. The exacerbations of the disease that occur in some patients after corticosteroid withdrawal usually respond well to the resumption of hormone therapy (sometimes at a slightly higher dose). The “scleroderm-like” features of SSTF (skin induration, impaired pulmonary diffusion and reduced esophageal motility) are the worst treatments, although these manifestations may also diminish in the early stages of the disease.
Lack of clear development of the main symptoms of NWPC after administration of corticosteroids is a reason for including long-term immunosuppressants, azathioprine, methotrexate or cyclophosphamide, into therapy.
Forecast
NWPC is considered relatively favorable. According to J. Wolfe et al., Who summarized the observations of more than 300 patients with a disease duration from 1 year to 25 years (average duration of 7 years), the mortality rate was only 7%. The causes of death were renal failure, damage to the lungs, myocardial infarction, colon perforation, brain hemorrhage, infection. In a number of patients with SSTP, persistent remissions have been described for several years, not only against the background of small maintenance doses of corticosteroids, but also without them.
There are also skeptic considerations about the favorable course and prognosis of the FTA. In particular, it is emphasized that in most of the works, the materials are analyzed mainly retrospectively. With this approach, of course, only surviving patients are evaluated, which obviously overstates the result.
When comparing patients with SLE itself and NWPC patients with “lupus” traits, attention is paid to the fact that the best prognosis in the second group is actually associated with the rarity of severe kidney damage in these patients. In this regard, it is suggested that the basis of a more favorable prognosis for FHDFs is based on the features of autoimmunization with nuclear components, resulting in antibodies not pathogenic to the kidneys to native DNA (so typical of classic SLE), but much more inert in this respect to antibodies to the nRNA, inherent to the FTAA.
R. Venables. He believes that the idea of a good prognosis and a favorable reaction to therapy during FHTC did not stand the test of time. It is emphasized, in particular, that the mere presence of antibodies to nRNA in patients with systemic scleroderma, dermatomyositis, and even SLE does not mean, in contrast to previous ideas, a more favorable course of the corresponding diseases compared to patients without these antibodies.
In conclusion, it should be recognized that, despite the many publications about the NWPC as an independent nosological unit, this issue cannot be considered finally resolved. Over time, the criteria for this disease, considered the most important and clear (the obligatory presence of antibodies to nRS, a good response to therapy, a relatively small kidney damage, a favorable prognosis), are not so strict. It is noteworthy that the diagnosis of SSTPs, which is very frequent in the late 70s and early 80s, is now rather the exception, indicating that overdiagnosis has occurred. There is a definite tendency to diagnose the primary DBST, the symptoms of which predominate. Nevertheless, the forms of FHCC typical in their clinical and immunological manifestations actually exist (although not so often). Apparently, they should be considered as one of the relatively natural variants of combined forms of DBST.